Improving health
through innovative reimbursement strategies
Our viewpoint
1 July 2022
Health economics and outcomes research (HEOR) is making important contributions to healthcare reimbursement strategies, using data and analytics to support innovative models that incorporate different elements when valuing healthcare interventions.
But the issues are complex, and translating theory to practice, a specialty of LCP, requires considerable expertise and an in-depth understanding of the issues involved.
The traditional methods of evaluating healthcare interventions are based on costs and patient-centred outcomes. For instance, in England and Wales, NICE (the agency that determines whether a healthcare intervention is clinically and cost effective enough to recommend for NHS use) recommends economic evaluation of healthcare interventions to assess:
- costs from an NHS and Personal Social Services (PSS) perspective; and
- health outcomes from a ‘direct to the patient perspective’.
However, these perspectives do not fully capture the value that interventions in certain contexts can offer, for instance interventions in the antimicrobial resistance and vaccine spaces could have broader societal value beyond NHS costs and outcomes directly linked to the patient.
A more comprehensive model is needed
One example of how we might look at the potential value elements of healthcare interventions is through the ISPOR Value Flower, which was established by an ISPOR Special Task Force in 2018[1] (Figure 1).
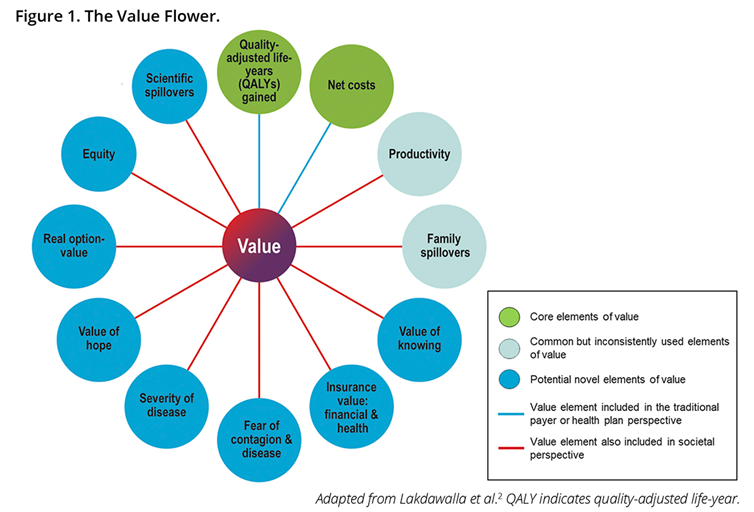
The ‘petals’ of the ISPOR Value Flower outline the types of broader value that could be derived from a healthcare intervention. The petals can be defined as:[2]
- Quality adjusted life years - a health outcome metric calculated by: Life years gained x Quality of life weighting (typically measured via a validated questionnaire).
- Net costs – these will be the cost savings the intervention brings net of the cost of implementation.
- Productivity – often considered as loss of ability to work, there are two main schools of thought in how to value this: the human capital and the friction cost approach.
- Family spillovers – how family members are affected by a patient’s condition. Relatives may need to spend time looking after the patient or, alternatively, a patient may no longer be able to care for family members.
- Value of knowing – the additional value of being able to predict (via e.g a diagnostic) who will respond well to a new treatment, new value is derived from this knowledge.
- Insurance value – the value of an intervention in preventing or mitigating impacts of adverse risk events.
- Fear of contagion and disease – also known as transmission value and applicable to infectious diseases, this is the value in preventing onwards transmission to a new person.
- Severity of disease – a greater value may be derived from an intervention that treats more severe conditions.
- Value of hope – the value of the patient risk profile; there is a trade-off between a treatment that has a mild to moderate effect on many people (a risk averse individual may value this higher) compared to treatment that has a strong effect on fewer people (a risk tolerant individual may value this higher).
- Real option value – the value of benefitting from future technologies and interventions due to additional life years gained.
- Equity – costs and QALYs are often viewed as averages per person that do not take equity or sociodemographic factors into account. There has been a suggestion that equity could be factored into economic evaluations through distributed cost effectiveness analysis.
- Scientific spillovers – value when one innovation is shown to work that eases the development of other interventions.
Some petals may contribute more than others under particular circumstances, while some may only be relevant to specific contexts. The NICE evaluation model only incorporates the two green petals, QALYs and Net costs.
Returning to the examples of antimicrobials and vaccines, the value of these may differ to those of other medicines because they may help to reduce transmission and have applications across the therapeutic spectrum. Antibiotics, for example, are critical to the lives of those who are taking immunosuppressant drugs and those with surgical site infections, and have a number of other uses where there are no alternative courses of action.
Vaccines demonstrated their societal value during the Covid-19 pandemic, precipitating changes in health policy in England that ended lockdowns and re-opened the bricks-and-mortar economy, both associated with greatly increased productivity. Yet these elements of value would be ignored if only taking the traditional NHS and PSS perspective. Disease severity is another important element. In what is perhaps the most significant move to date towards application of additional elements of value by a recognised reimbursement body, NICE has produced guidance on how to factor severity of disease into cost-effectiveness analysis. The guidance shows how health outcomes (QALYs) should be weighted according to the age of the population being affected by the intervention. NICE severity of disease guidance is a clear signal of intent to explore and apply at least some of the additional elements.
However, much of the other work on the Value Flower remains theoretical, with some debate as to whether the additional elements are needed at all. Some economists have argued against inclusion, preferring to stick with the status quo of cost and outcome assessment in health technology assessments (HTA). They argue that incorporating additional elements adds complication and uncertainty to what can already be complicated and uncertain. But what should be done when status quo leads to market failure?
The current HTA system is not designed to incentivise manufacturers to invest in R&D to identify new antimicrobials, consequently the demand for products (high) has been de-linked from innovative supply (low). In economic terms this is market failure, and in healthcare terms the consequences could be severe.
This de-linkage between supply and demand has occurred due to the peculiarities of how we use antimicrobials. Good stewardship of antimicrobials guides clinicians to use these medicines as last resorts (to reduce the chance of antimicrobial resistance), this translates to low sales and profit relative to other classes of medicine for the manufacturer.
This has led to less R&D and hence a slow decline over recent decades in the number of successful antimicrobials reaching the market. Using additional elements of values, and/or innovative reimbursement mechanisms such as outcomes-based agreements, may help the system to address market failures on the supply side, incentivising production of these critically important medicines.
Despite some voices of concern, using additional elements of value may help to bridge the gap between traditional interpretations of value (costs from an NHS and PSS perspective) to the broader value that certain interventions bring to society. Yet there remains a huge amount of work to do if we want to put a quantitative practical framework on each of the value elements.
The LCP Health Analytics team is well positioned to help translate the ISPOR Value Flower from economic theory to economic application, and has been working on several of the elements for some time. LCP’s actuarial heritage and health analytics expertise lends itself particularly well to elements such as the Insurance value of interventions.


