Echoing patient concerns:
GP survey exposes persistent challenges in primary care
Our viewpoint
25 July 2023
Demand and complexity in primary care is increasing, driven by a mixture of workforce challenges and a rising number of patients living with chronic, multi-morbid diseases requiring long-term support.
Digital channels for appointments are recognised as increasingly important for managing GP workload and improving access, but questions remain surrounding their effectiveness and ability to meet patients’ needs.
The GP Patient Survey is an independent patient experience survey run on behalf of NHS England every January to April. We dig into the results from the 2023 survey in this blog to understand the latest national and local trends in patient experience, shedding light on how the healthcare sector can enhance primary care delivery across the UK.
Access to care
Survey results from previous years displayed a downward trend in overall patient experience between 2018-20; this was followed by a slight improvement in 2021 before a marked downturn in 2022. The 2023 results show a further drop across the following metrics:
- Overall patient experience of GP practice;
- Experience making an appointment;
- Ease of getting through to a practice by phone.
The drop in overall satisfaction strongly correlates with increasing patient dissatisfaction with the accessibility of GP services. According to the latest data, only half of survey respondents find it easy to reach their GP practice over the phone, a drop from 68% in 2021. Similarly, patients’ experience with appointment scheduling has also worsened. Today, just 54% of respondents reported a good experience, compared to 71% two years ago.
Figure 1: Reported experience of GP practices and access is worsening
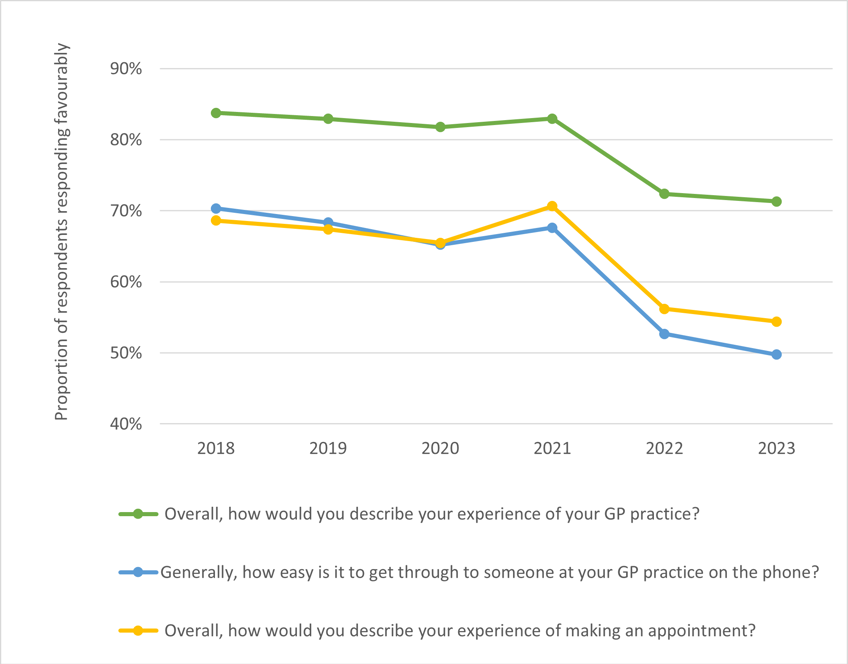
Abbreviations: GP, general practice. Source: GP Patient Survey 2023
The evolving nature of appointments could be contributing to the decline in reported patient satisfaction. A large proportion of patients report being offered telephone consultations instead of traditional face-to-face visits. In some cases, this might reflect patient preference; however, only 59% of patients were offered a choice of type of appointment in 2023, compared to 69% in 2021 (Figure 2).
Figure 2: The types of appointments offered by GP practices is evolving
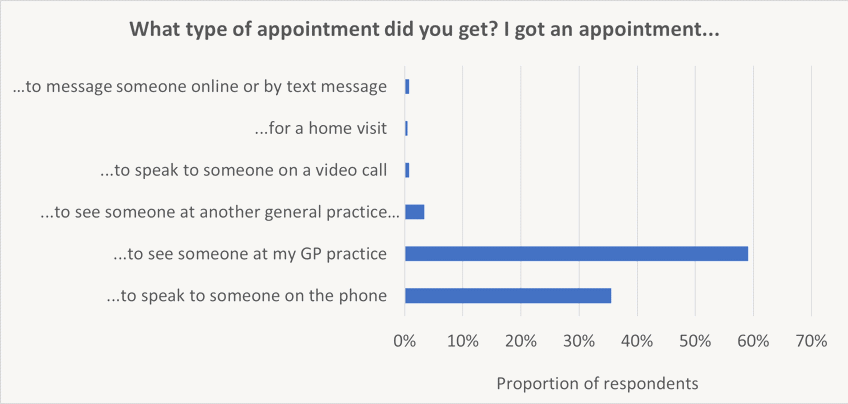
Abbreviations: GP, general practice. Source: GP Patient Survey 2023
Regional variation in patient satisfaction
Interestingly, there is substantial disparity in satisfaction scores nationwide. The Midlands and the South-East stand out as the regions where fewest individuals deem their experience as "good", with lowest scores observed in Bedfordshire, Luton and Milton Keynes ICS, Black Country ICS and Birmingham and Solihull (all 63%). On the other hand, the South-West records the highest proportion of patients (78%) reporting a good experience, with the highest overall score achieved by One Gloucestershire ICS (80%). Similar trends are evident when analysing the proportion of telephone/remote appointments compared to face-to-face visits, with 40% of all appointments conducted over the telephone in London and 38% in the South-East. The proportion of telephone appointments is lowest in the North-East and Yorkshire (31%). Regions with the lowest patient satisfaction are generally those with the highest proportion of telephone consultations. While remote appointments have the potential to enhance GP efficiency and improve access, especially in more rural regions, their current implementation appears to be problematic and may contribute to growing health inequalities.
Figure 3: There is considerable variation in patient experience across ICBs
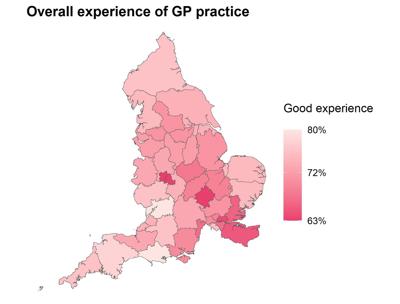
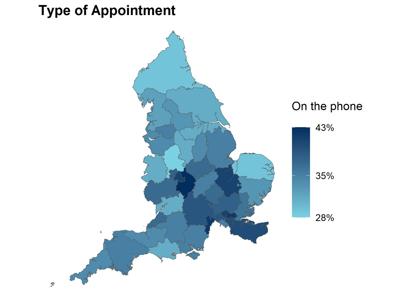
Abbreviations: GP, general practice; ICB, integrated care board. Source: GP Patient Survey 2023
Figure 4: There is a correlation between the number of phone appointments and overall GP experience
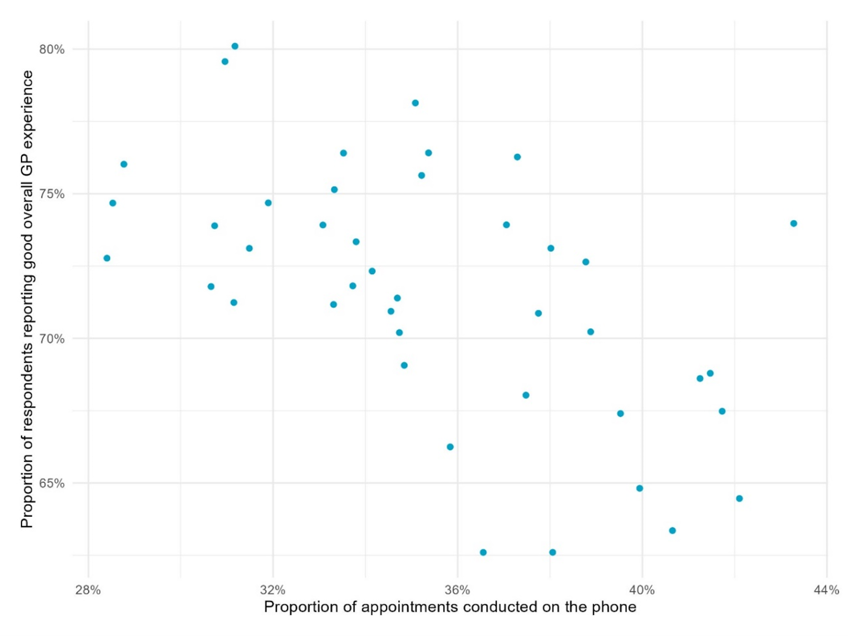
Abbreviations: GP, general practice. Source: GP Patient Survey 2023 Figure 4 illustrates the correlation between appointment type and the overall experience of the GP practice. It reveals that practices with the lowest proportions of phone appointments have the highest proportions of individuals rating their overall GP experience positively.
The survey findings seem to reflect broader public sentiment surrounding the NHS, shedding light on staffing problems that have increasingly plagued the primary care sector. A shrinking GP workforce compared to ten years ago adds fuel to these concerns.
Transforming our primary care model
To tackle these issues, the NHS recently outlined a delivery plan for recovering access to primary care, which, among other things, involves bolstering the role of pharmacies. Pharmacies will be authorised to prescribe medication, including antibiotics and antivirals. This move is predicted to free up to an estimated 10 million appointments annually once scaled to a national level. The success of this strategy, however, is not guaranteed, as it leans heavily on patients first diagnosing their condition accurately and second, opting for pharmacies as their primary healthcare recourse. In addition, whilst a step in the right direction, when viewed in the context of approximately 340 million appointments conducted every year, this measure is far from the comprehensive solution required.
A more promising step is the increase in the number of training places for GPs by 50% by 2031, included in the NHS’s first-ever long-term workforce plan. This could have a profound impact, increasing the number of new trainees each year from 4,000 to 6,000. The number of GPs working in the NHS is set to increase to 53,000 FTE by 2036/37, representing a 46% increase from the current numbers. The fruits of this strategy, however, are several years away.
A reason to be optimistic
Despite the challenges, it’s not all doom and gloom in primary care. The 2023 GP patient survey results show that patients’ rating of the care received remained high, with 93% saying they had confidence and trust in the healthcare professional they saw at their last appointment (unchanged since 2022) and 84% saying they were treated with care and concern (up from 83% in 2022). Often referred to as the backbone of the NHS, it is welcome to see that the current issues in primary care appear to lie in quantity, not in the quality-of-care patients receive.